The Genomics Paradox: Proven Technology, Limited Access
Author: Peechu Sachdeva, Market Strategy Lead, Axia Medicine
Published by Axia Medicine | November 2025
This article is part of a series.
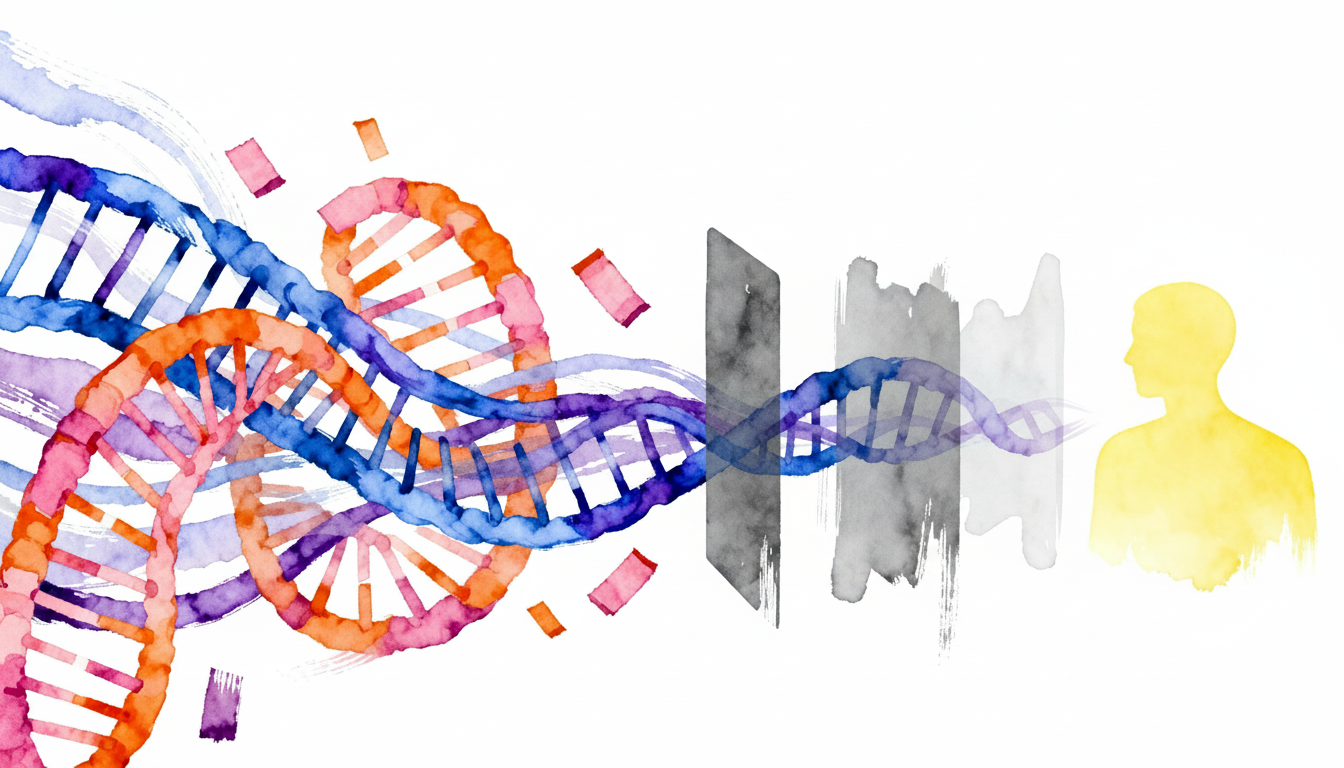
For much of its history, genomics was viewed as a resource for research rather than clinical practice. That distinction no longer holds. Advances in sequencing technology, the rise of multimodal data and the mainstream adoption of AI are propelling genomics into healthcare, where its impact is measured not in publications, but in improved lives.
In 2025, the discussion has finally moved from "read length” to life expectancy. The focus is now on how genomic insights can meaningfully improve diagnosis, treatment, and prevention within clinical settings.
Genomics Moved Into the Clinic
Today whole-genome sequencing is used in neonatal care to deliver rapid diagnoses for rare diseases, sparing families years of uncertainty and enabling timely treatment. In oncology, biomarker-driven approaches are reshaping how trials are designed and how therapies are matched to patients, improving both efficiency and outcomes. At the population level, programs such as All of Us are linking genomics with environmental and clinical data to model chronic disease trajectories.
What once required years of international efforts and billions of dollars can now be accomplished in a few hours for hundreds of dollars in a small laboratory. “Genomic medicine” is no longer a buzzword or a distant prospect; it is here, in the clinic, today.
Innovation Outpaces Integration
DNA sequencing has kept evolving across time, space and money. While Illumina ’s acquisition of Edico and software specialists like Sentieon unlocked ultra-fast variant analysis, a third-generation entrant like Oxford Nanopore Technologies has pioneered portable sequencing technologies. A decade ago, the $1,000 genome was utopian; Ultima Genomics now makes a credible case for the “$100 genome”. Organizations like PacBio , Element Biosciences and BGI/ Complete Genomics keep competing in a global DNA sequencing ecosystem which is still largely shaped by one dominant incumbent.
Still, especially thanks to Illumina’s Novaseq technology, we enjoy unprecedented capacity in producing “omics” data. The availability of hundreds of petabytes of Omics data is remarkable, yet mostly limited to biomedical research. The greater opportunity for the industry has always been in real world applications; as we see in Precision Public Health, for a consumer, nothing gets more real than our own health.
For genomics to deliver sustained value, it must be embedded within healthcare systems in ways that respect clinical governance, preserve patient trust, and align with how care is delivered over time.
Turning Discovery Into Value
The case for embedding genomics into everyday clinical workflows is compelling for patients, clinicians, and industry alike.
For pharmaceutical companies, the economics are pressing: the average cost of bringing a therapy to market exceeds $2.6 billion, yet nine out of ten trials fail. Genomics has been rapidly updating this equation, enabling more precise patient stratification and trial designs that improve efficiency and probability of success. Examples such as Vertex Pharmaceuticals’s cystic fibrosis therapies, which generated nearly $9 billion in 2023 and are projected for further growth, show the scale of opportunity when genomic insights guide development.
For care-providers and patients, the benefits are tangible. Earlier and more accurate diagnoses, fewer trial-and-error prescriptions, and predictive models such as polygenic risk scores offer new opportunities for prevention and personalised care. These advances are most effective when genomic data is interpreted alongside clinical history, environmental context, and longitudinal care relationships.
The Revolution will not be Normalized
When we think about Precision Medicine’s “4Ps” - Predictive, Preventive, Participatory and Personalised, it’s clear that just generating vast amounts of data is not going to move the needle for the general public.
When we look at the big picture, genomic medicine is still removed from most patients. As the next article, The Multimodal Shift examines, abundant data does not guarantee meaningful access. Without appropriate governance, consent frameworks, and integration with clinical systems, even the most comprehensive genome lacks the context required for safe and meaningful use.
National scale initiatives for health data research, like UK Biobank, Finngen and All of Us show what is possible at population scale. However, these initiatives effectively pilot for broader adoption of Genomic Medicine; and 10 years after Genomics England’s creation, virtually all advanced economies are still far from enabling full access to genomic innovation.
Even with a $10 genome, Genomic Medicine comes with costs and challenges in terms of infrastructure, data governance, talent and legacy technology stacks. The later article Precision Public Health expands on this systemic failure, showing how fragmentation across health records, registries and databases leads to preventable errors, missed diagnoses, and stalled research. This reflects the complexity of protecting patients while enabling innovation.
To make genomic medicine equitable and effective, a different approach is needed. One that recognizes clinics and health systems as long-term stewards of patient data, trusted intermediaries of consent, and essential partners in research.
Clinical data gains its value through continuity of care. Longitudinal relationships, multimodal context, and ethical oversight are what allow genomic insights to translate into real-world impact. Research collaboration works best when it is built on these foundations, not around them.
Tomorrow’s Medicine, Built Today
The next phase of the genomic revolution is not about amassing more data. It is about creating trusted frameworks that allow data to be used responsibly, transparently, and with clear purpose. Patients, industry, and health systems all stand to gain. But as we see later in the series, if we want to truly bridge the gap from small-scale biomedical research and national benefit, a new approach is needed; the infrastructure Precision Medicine has been waiting for, which supports collaboration rather than bypassing it.
At AXIA, we believe the future of precision medicine depends on enabling patients and clinics to participate together in ethical research partnerships. By supporting consent-driven, purpose-specific access to multimodal and longitudinal data, we aim to help translate genomic discovery into lasting clinical and societal value.
References
Anaya, J.-M., Herrán, M. and Pino, L.E. (2025). Challenges and opportunities for precision medicine in developing nations. Expert Review of Precision Medicine and Drug Development, 10(1), pp.1–15. doi:https://doi.org/10.1080/23808993.2025.2505796.
Fountzilas, E., Tsimberidou, A.M., Vo, H.H. and Kurzrock, R. (2022). Clinical trial design in the era of precision medicine. Genome Medicine, 14(1). doi:https://doi.org/10.1186/s13073-022-01102-1.
Glynn, P. and Greenland, P. (2020). Contributions of the UK biobank high impact papers in the era of precision medicine. European Journal of Epidemiology, 35(1), pp.5–10. doi:https://doi.org/10.1007/s10654-020-00606-7.
Handra, J., Elbert, A., Gazzaz, N., Moller-Hansen, A., Hyunh, S., Lee, H.K., Boerkoel, P., Alderman, E., Anderson, E., Clarke, L., Hamilton, S., Hamman, R., Hughes, S., Ip, S., Langlois, S., Lee, M., Li, L., Mackenzie, F., Patel, M.S. and Prentice, L.M. (2023). The practice of genomic medicine: A delineation of the process and its governing principles. Frontiers in Medicine, 9. doi:https://doi.org/10.3389/fmed.2022.1071348.
Hasanzad, M., Sarhangi, N., Naghavi, A., Ghavimehr, E., Tavangar, S.M., Chimeh, S.E., Larijani, B. and Meybodi, H.R.A. (2021). Genomic medicine on the frontier of precision medicine. Journal of diabetes and metabolic disorders, 21(1), pp.853–861. doi:https://doi.org/10.1007/s40200-021-00880-6.
Manickam, K., McClain, M.R., Demmer, L.A., Biswas, S., Kearney, H.M., Malinowski, J., Massingham, L.J., Miller, D., Yu, T.W. and Hisama, F.M. (2021). Exome and genome sequencing for pediatric patients with congenital anomalies or intellectual disability: an evidence-based clinical guideline of the American College of Medical Genetics and Genomics (ACMG). Genetics in Medicine, 23(11). doi:https://doi.org/10.1038/s41436-021-01242-6.
Modi, A., Vai, S., Caramelli, D. and Lari, M. (2021). The Illumina Sequencing Protocol and the NovaSeq 6000 System. Methods in Molecular Biology (Clifton, N.J.), [online] 2242, pp.15–42. doi:https://doi.org/10.1007/978-1-0716-1099-2_2.
Moore, D.C. and Guinigundo, A.S. (2023). Biomarker-Driven Oncology Clinical Trials: Novel Designs in the Era of Precision Medicine. Journal of the advanced practitioner in oncology, 14(3), pp.9–13. doi:https://doi.org/10.6004/jadpro.2023.14.3.16.
National Human Genome Research Institute (2017). DNA Sequencing Costs: Data | NHGRI. [online] Genome.gov. Available at: https://www.genome.gov/about-genomics/fact-sheets/DNA-Sequencing-Costs-Data.
Purkayastha, D., Agtarap, K., Wong, K., Pereira, O., Co, J., Pakhale, S. and Kanji, S. (2023). Drug-drug interactions with CFTR modulator therapy in cystic fibrosis: Focus on Trikafta®/Kaftrio®. Journal of Cystic Fibrosis, 22(3). doi:https://doi.org/10.1016/j.jcf.2023.01.005.
Satam, H., Joshi, K., Mangrolia, U., Waghoo, S., Zaidi, G., Rawool, S., Thakare, R.P., Banday, S., Mishra, A.K., Das, G. and Malonia, S.K. (2023). Next-Generation Sequencing Technology: Current Trends and Advancements. Biology, [online] 12(7), p.997. doi:https://doi.org/10.3390/biology12070997.
Sperber, N.R., Carpenter, J.S., Cavallari, L.H., J. Damschroder, L., Cooper-DeHoff, R.M., Denny, J.C., Ginsburg, G.S., Guan, Y., Horowitz, C.R., Levy, K.D., Levy, M.A., Madden, E.B., Matheny, M.E., Pollin, T.I., Pratt, V.M., Rosenman, M., Voils, C.I., W. Weitzel, K., Wilke, R.A. and Ryanne Wu, R. (2017). Challenges and strategies for implementing genomic services in diverse settings: experiences from the Implementing GeNomics In pracTicE (IGNITE) network. BMC Medical Genomics, 10(1). doi:https://doi.org/10.1186/s12920-017-0273-2.
Sun, D., Gao, W., Hu, H. and Zhou, S. (2022). Why 90% of clinical drug development fails and how to improve it? Acta Pharmaceutica Sinica B, [online] 12(7). Available at: https://pmc.ncbi.nlm.nih.gov/articles/PMC9293739/.
The All of Us Research Program Investigators (2019). The ‘All of Us’ Research Program. New England Journal of Medicine, [online] 381(7), pp.668–676. doi:https://doi.org/10.1056/nejmsr1809937.
Xiang, R., Kelemen, M., Xu, Y., Harris, L.W., Parkinson, H., Inouye, M. and Lambert, S.A. (2024). Recent advances in polygenic scores: translation, equitability, methods and FAIR tools. Genome Medicine, [online] 16(1). doi:https://doi.org/10.1186/s13073-024-01304-9.
Yu, H.W.H. (2016). Bridging the translational gap: collaborative drug development and dispelling the stigma of commercialization. Drug Discovery Today, 21(2), pp.299–305. doi:https://doi.org/10.1016/j.drudis.2015.10.013.